Special Report
Investigation: Untold Story Of Nigeria’s Oil Producing Communities Battling Poor Health System

Access to quality healthcare is one of the nightmares of communities in Ilaje local government area of Ondo State. Despite the revitalization plan for Primary Health Centers in Nigeria, oil-producing communities in Ilaje suffer neglect. In this report, ADESOLA IKULAJOLU risked a journey to visit different Primary Health Centers in ILAJE and document the plights of the residents.
When Festus Monday, 25years-old visited Ilaje community, a coastal area in Ondo State, in November 2020 during the COVID-19 pandemic, he was expecting to see residents comply with the precautionary measures of wearing face masks, physical distancing, and use of hand sanitizer. With disappointment all over his face upon discovering that he was the only person wearing a face mask around during his stay in the area, Festus was compelled to pull off his face mask.
“I was surprised to see people not bothered about COVID-19 but when I saw that I was the odd one, I pulled off my face mask so they wouldn’t stare at me like a stranger.”
The communities he visited were Mese, Gbagira, Molutehin, Odofado, Ilowo, Ilepete, Oju-Imole, Awoye, Obenla, Ogungbeje, and Ayetoro; they are oil-producing areas on the riverine area of Ondo State which also connects to the Atlantic Ocean.
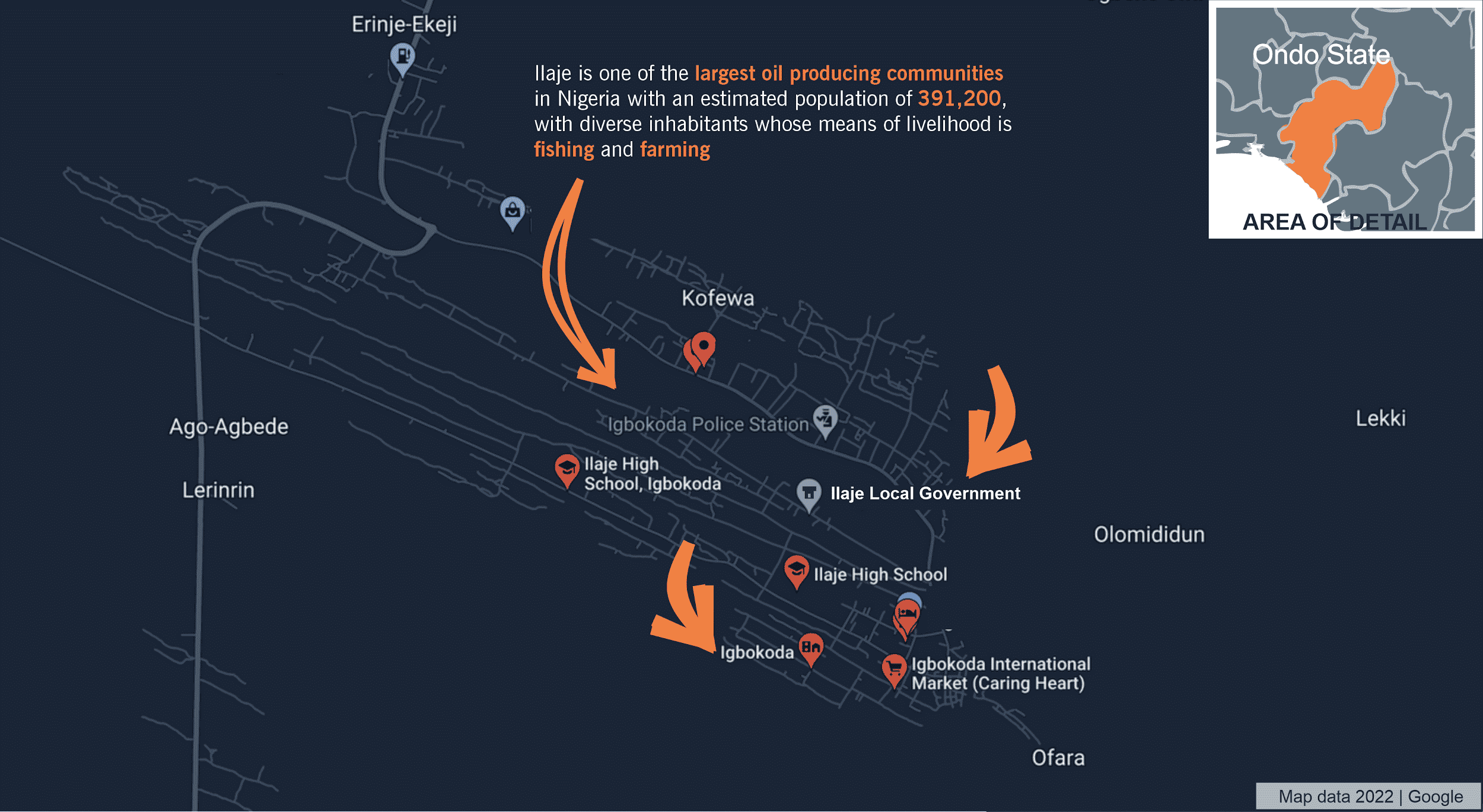
Ilaje visual illustrated map
As at the end of November 2020, figures according to the National Center for Disease Control (NCDC) showed that Nigeria had 67,557 cases, 1173 deaths and 63,282 discharged; Ondo State recorded 1,728 cases at that time. It was an increasing number, yet Festus said residents of the Ilaje communities he visited were not bothered “neither were they complying with the safety guidelines and these communities don’t even have hospitals nor functional health facilities.”
“When the world was battling COVID-19, these communities in Ilaje had no access to health information. All the health centers in that area are in dilapidated form, they are not working. How would they even detect any health disease? The people are the ones treating themselves with traditional medicine since there is no health personnel to treat them.”
“They have abandoned all the health centers, they can not treat ordinary sickness and not all of them will have money to travel to a hospital in another place to receive medical treatment. Who knows how many people might have even died from this ugly situation besieging the people of these communities,” Festus lamented to this reporter.
Twenty months later, in the company of Festus, this reporter visited some of these Ilaje communities battling poor health systems. Ilaje is one of the largest oil-producing communities in Nigeria with an estimated population of 391,200, with diverse inhabitants whose means of livelihood are fishing and farming.
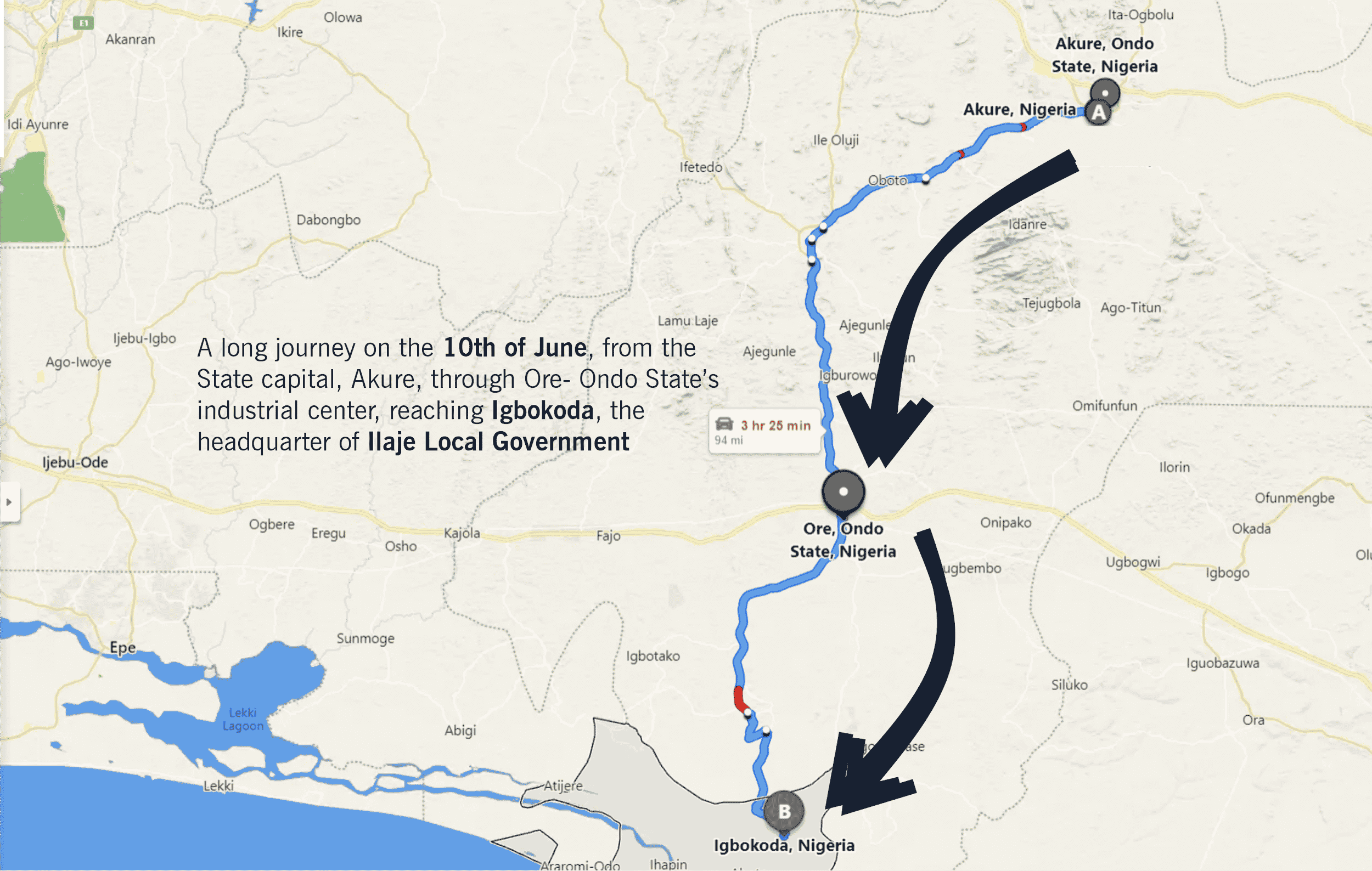
From what began with a long journey on the 10th of June, from the State capital, Akure, through Ore- Ondo State’s industrial center, reaching Igbokoda, the headquarter of Ilaje Local Government. A few hours from Igbokoda, another journey began from Ugbo-Nla, from where all visitors and inhabitants can access the communities using boats. All around the busy seashore were children, women, and men going about their businesses while the boats were loading and offloading passengers.

This path leads to the primary health center in Ilepete and Odu-Oretan in Ilaje. Photo Credit: Adesola Ikulajolu – 11/06/2022
Staff Shortage, No Medicine
Tophas, in his early 30s, visited the health center in Molutehin community to complain about a condition he was battling but he was referred to the hospital in igbokoda. He was neither given medicines nor asked to undergo any form of test to ascertain what he was complaining about. Since Tophas was unable to visit the hospital they referred him to because of the distance, he resorted to self-medication.
“When we go to the health center, they refer us to Igbokoda. The health center in Odu-Oretan has no doctor. The one at Molutehin, once they work small, they close. If not for God saving us and that our people here are strong, they would have been dying untimely,” Tophas said.

Abandoned Primary Health Center in Odu-Oretan community taken over by stagnant water and left in dilapidated condition
On June 11, this reporter visited the Molutehin PHC in the company of Festus who went to complain about chest pain and stomach upset resulting from the borehole water he drank. The only nurse available on duty that day at the health center asked Festus to sit for more than ten minutes while she attended to another patient. There were no other health officials at the health center.
When Festus requested the drug to suppress his pain, the young female nurse identified as Odunayo said “there is no drug on the ground but I will write the prescription for you to buy, the doctors only come here once a while.” There was also no vitamin C to give Festus.
Josiah Olusegun is one out of the many residents of Ilepete community who said they “can not rely on the health center because they will say no drug.When we go to this health center to complain, they will say the government did not give them drugs, and sometimes we won’t meet anyone to attend to us.”
This reporter visited Ilepete Primary Health Center located at the opposite side of the community with Festus disguised to be battling a sore throat. That evening, at the health center, there were two female nurses. After listening to his complaint of Festus, one of the nurses referred him to Igbokoda for an X-ray.
“No doctor here, we only have nurses. There is no medicine that we give you because only X-ray can tell us what to do and that will be in Igbokoda,” Ms. Pelumi, one of the nurses said.
Residents also revealed that they are at the mercy of “quack” health attendants and chemists within the community. Meanwhile, communities like Mese, Gbagira, Awoye and Odofado also have similar predicaments.
“There is no hospital here to treat anyone. We are always running helter-skelter to save ourselves. Those who have money struggle to take their people to Igbokada and some even die before getting to Ugbonla for emergency treatment. The distance between Igbokoda is too far from us,” Mr. Monday Adebanwo, a resident of Gbagira lamented.
Data from the World Health Organisation (WHO) stated that the patient-to-doctor ratio in Nigeria is 2500:1 which is four times higher than the WHO recommendation of 600:1.
In Ilowo And Odu-Oretan: Facilities Underlock, Doctors Unavailable

Abandoned Primary Health Center in Odu-Oretan community taken over by stagnant water and left in dilapidated condition
The PHC at Odu-Oretan community is surrounded by stagnant water and bushes. At the entrance of the health center is a wooden walkway that leads to the door of the deserted building, but the facility was under lock with no health officials available.

A source who spoke to this reporter said the doctor, one Mr. Blessing Ogungbeje who formerly worked at the PHC had left. The facility is under lock with no visible equipment. This reporter also observed an abandoned building already collapsing beside the Odu-Oretan PHC- the source said it was to house a new health facility but was neglected halfway.
“Only one doctor was here, all the nurses have left because they said they cannot survive in the community. No doctor here again and they locked the government health centre. People only go to get drugs personally,” the source told this reporter.
At Ilowo, the facility housing the Primary Health Center has been outgrown by bushes and put under lock. A resident said the doctors are not always around and they have to resort to self-medication. When this reporter visited the PHC, there were no health officials available.
Mrs Adeyin Ibiola lamented that the closure of the Ilowo PHC is making other residents seek after “quack doctors” and traditional means in the community while those who have money travel to Igbokoda hospital on their own.
“If our children have any sickness, we apply traditional means, since the health center is locked and doesn’t even have enough medicines. Pregnant women go to the health center, but most of them resort to the traditional way. Anyone who has the money will quickly go to Igbokoda. Hospital is not supposed to close. What if there is an emergency”

One of the buildings where residents of Ilepete and neighbouring communities receive traditional health. Pregnant women also deliver their babies here. Photo credit: Adesola Ikulajolu – 10/06/2022
Failed PHCs’ Revitalisation Plan
President Muhammadu Buhari, in January 2017, flagged off a scheme to revitalise 10,000 PHCs across the country to create qualitative and affordable health services for poor Nigerians. The revitalisation plan was to make at least one PHC fully functional in each of the wards across 109 senatorial districts of the country through the National Primary Health Care Development Agency (NPHCDA).
The NPHCDA guideline requires that a standard PHC should have a labour room, office and staff quarters, well open ward, children and female wards, an ambulance for referrals, preventive and basic curative care, drugs and equipment for immunisation. But the PHCs in Ilowo, Ilepete, Molutehin, Odu-Oretan, Gbagira and Odofado are far from these requirements.
This investigation revealed that despite the annual allocations of the Basic Health Care Provision Fund (BHCPF) to strengthen, provide access and emergency medical treatment, PHCs are largely under-equipped and nonfunctional. The federal government initiated a N28 billion health fund in December 2017, to revitalise PHCs, but the impact of such allocation is not felt in Ilaje communities.
In Ondo State, there are a total of 811 health facilities. Of this number, 95 % (769) are Primary Health Care facilities, 40 are Secondary Health Care facilities and 2 are tertiary healthcare facilities. Of the 769 PHC facilities, 60% (460) are public owned. The remaining 309 or 40% are private providers. At the secondary health care level, 48% (19 ) of 40 health facilities are public owned while 21 (52%) are privately owned. The two tertiary health facilities in the State are public owned.
Ilaje has 31 health facilities available with 26 public-owned PHCs, 3 private-owned PHCs, 1 public-owned secondary health facility and 1 private-owned secondary health facility making it rank 11th out of 18 LGAs.
In a report published by SBM Morgen, the 36 states spent an average of 4.65% of their budgets on healthcare in 2021 which is a decrease to 11% in 2020. Ondo State was among the only two states whose healthcare budget was more than 10% in 2021 which is proof of Governor Rotimi Akeredolu’s commitment to providing access to health, but the impact is not reflected in some Ilaje communities.
Bababo Ikuemonisan, an advocate and indigene of Ilaje has challenged the Ondo State government to come to the aid of the people and not neglect their communities in terms of healthcare.
“Lack of a standardized health system for the riverine people in Ilaje will necessitate rushing of sick patients to faraway Owo, Akure or Ondo. Some of these patients die before reaching the hospitals in the hinterlands. A state-of-the-art hospital should be built where people can access and all PHCs should be well equipped,” he said.
We prefer the traditional birth method- Women
According to UNICEF data, Nigeria has an under-five mortality rate of 113.8 per 1,000 live births; the infant mortality rate is 72 per 1,000 live births; only 35% of children under age 5 have their births registered.
World Health Organisation (WHO) highlighted that Nigeria accounts for over 34% of global maternal deaths. Figures show a maternal mortality rate of 576 per 100,000 live births, the fourth highest in the world.
Atike Faroye is one of the oldest traditional birth attendants (Agbebi) in Ilepete community, pregnant women from nearby communities visit him for childbearing or during pregnancy complications. The over 70yrs-old man said he has delivered more than 400 births within and outside his community. Faroye lamented that he delivers more than four births in a week but some of them pay N500 while some cannot even afford it.
“I didn’t learn this work from anyone. There is traditional medicine we give pregnant women to help their pathways open and some will even give birth on the way since they have used their medicine well. The health centre here use to bring people to my place- they can not handle birth delivery because there are no midwives. At night, when they bring pregnant women, we deliver them here,” Faroye told this reporter.
When Mrs Adeyin wanted to give birth to her first child in her twenties, her preference was the traditional birth attendant due to her belief, what she inherited from her parents and the inaccessibility of health centres.
Another woman from Ogungbeje community told this reporter that “rather than go for antenatal care at the health centre, they prefer to visit the traditional birth attendants.”
She added that hardly will pregnant women decide to go to the health centre because of the fear of being neglected and mostly no means of transportation during emergencies.
This reporter observed that there were neither midwives in all of the health centres nor were there any ambulances to convey patients when there is an emergency.

We are not aware- officials react
The agency in charge of all the PHCs in Ondo State is the Ondo State Primary Health Care Development Board (OSPHCDB) with the aim to make quality basic health care available and accessible to every citizen regardless of their status. OSPHCDB is one of the Ministries, Departments and Agencies (MDAs) under the Ondo State Ministry of Health.
This reporter reached out to the Permanent Secretary of ONDOSPHDB, Dr Francis Akanbiemu, to confirm if he is aware of the findings that health facilities in Ilowo and Odu-Oretan are under lock.
“I am not aware of that, maybe you have to call the PCH coordinator. I oversee the local governments, we have over 600 health centers and there is no way I will be at all the places at the same time. The best person to call is the PHC in Ilaje – his name is Dr Ayelaje. There is no way I can confirm because I am not a machine, there is no way I can be in all the health centers at the same time- no health is supposed to be under lock and key. We have a PHC authority in Ondo state, each of them headed by the Medical officer, they are the ones that directly supervise what happens in those health facilities.”
He noted that he is not aware if the health facility in Odu-Oretan is under lock but highlighted that an investigation will be conducted.
Dr Francis added that after the investigation, “whoever is found wanting will be punished, we don’t cover anybody who does not do well. We have to document your findings because if we want to punish anybody for doing wrong, you have to provide evidence.”
In another conversation, the PHC coordinator in ILAJE through the Permanent Secretary revealed that the health facility in Ilowo has been taken over by OSOPADEC. But he was silent on the status of the Odu-Oretan’s facility.
The present condition of the Primary Health Center in Odu-Oretan is now locked and abandoned. Photo credit: Adesola Ikulajolu – 11/06/2022

“We don’t lock our facilities, what he made me to believe that the Ilowo PHC has been taken over by OSOPADEC and they refuse to work with the PHC authority. So the PHC authority is no longer incharge of the Ilowo health centre. We don’t lock our facilities, if you see anyone, just know that it is not under our care.”
The Director of Research, Planning and Statistics at the Ondo State Ministry of Health, Dr. Uche Odionyenma, also expressed his surprise over the locking and shortage of staff at the health centres.
“I am not aware. I was told during my trip that some PHCs are non-functional, I don’t know what that means but I wasn’t given the name. From this enquiry you are giving me, I will find out why exactly it is under lock or there is no staff or the building is collapsing, there must be a reason for locking such a place. The only way I can do this is to get across to the PHCDA. We will investigate this.”
When confronted with the issue of a shortage of staff at some of the PHCs in Ilaje, the Director of Nursing at OSMoH, Mrs Alice Ogundele noted that it is not only in those areas.
“It is all over. That is why the government keeps employing. An advert is out. Partners are helping too. We are trusting that things will be alright,” Mrs Alice said through SMS.
Access to quality healthcare is still a challenge, especially to the residents of the oil oil-producing communities in Ilaje. The government and concerned agencies must rise to salvage the situation to save the lives of these people with adequate medical infrastructures and revitalization of the PHCs.
This story was supported by the Africa Data Hub Community Journalism Fellowship.